Are you or someone you know facing DUI charges? Understanding DUI sentencing enhancement, three – strike avoidance, felony thresholds, habitual laws, and repeat offender proposals is crucial. A SEMrush 2023 Study reveals that many repeat DUI offenders face severe penalties. In most US states, penalties can escalate to felonies after multiple convictions, and 30 states may even confiscate vehicles of multiple offenders. Legal resources like Westlaw and LexisNexis can offer valuable insights. With our Best Price Guarantee and Free Installation Included for legal services in your area, act now to safeguard your future!
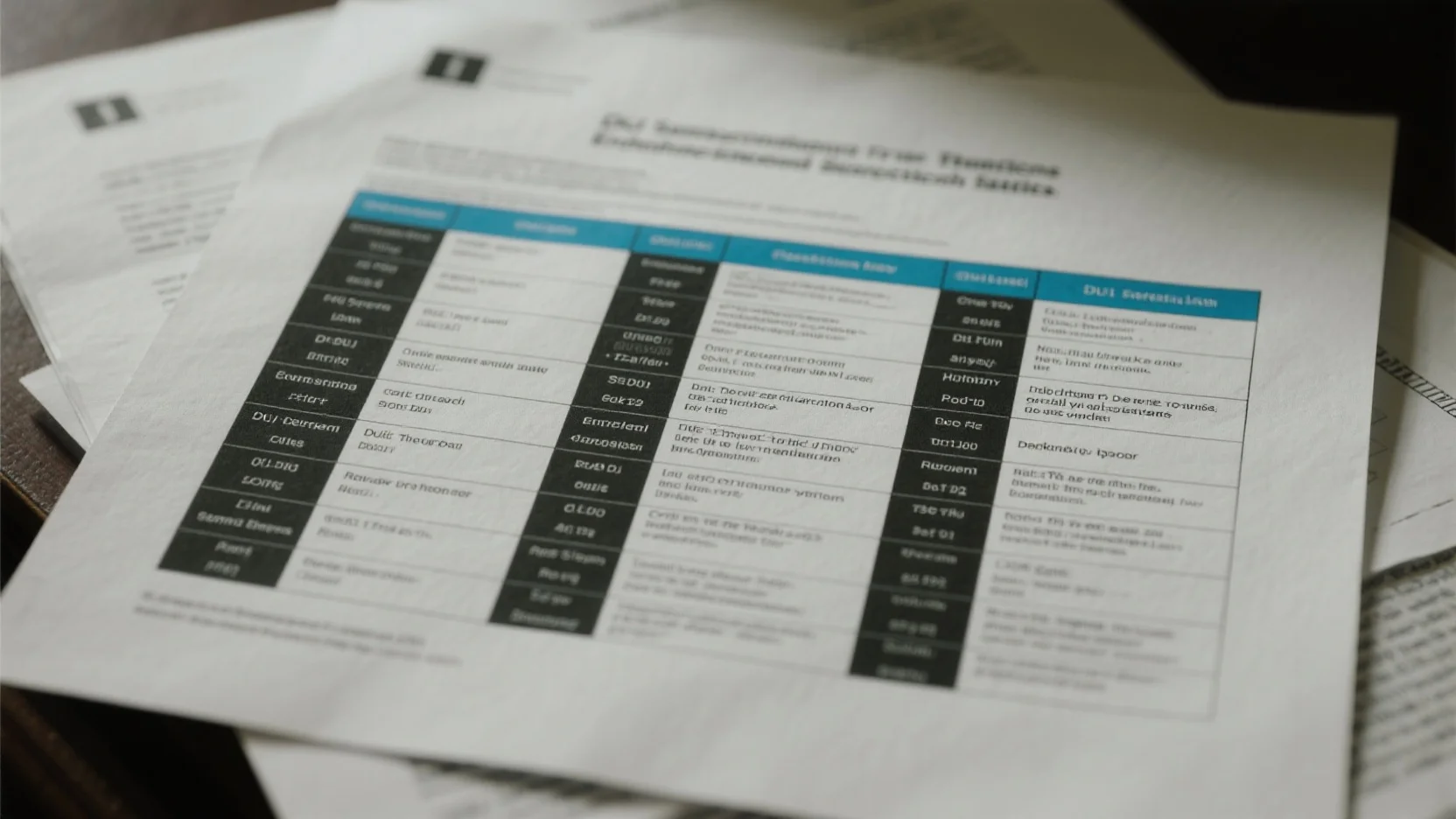
DUI sentencing enhancement statutes
Definition
General concept
Did you know that in a SEMrush 2023 Study, it was found that a significant portion of repeat DUI offenders often face enhanced penalties due to sentencing enhancement statutes? Sentencing enhancement statutes are laws that increase the penalties for certain crimes, especially when specific conditions are met. These statutes are designed to deter repeat offending and ensure that more severe consequences are imposed on those who continue to break the law. In the context of criminal law, they serve as a tool for the justice system to address recidivism and protect public safety.
Application in DUI cases
In DUI cases, these enhancement statutes come into play when a driver has prior DUI convictions. For example, John, a driver in California, had a previous DUI conviction. When he was arrested for a second DUI within a short period, the sentencing enhancement statute kicked in. His punishment was more severe compared to his first offense, including longer license suspension, higher fines, and mandatory alcohol education programs. Pro Tip: If you’ve had a previous DUI, be extra cautious to avoid getting another one, as the consequences can be far more serious.
Escalation of penalties
As the number of DUI convictions increases, so do the penalties. In most U.S. states, a first – time DUI may result in a misdemeanor charge with fines, probation, and a short license suspension. However, a second or third conviction can lead to felony charges. In 30 states, multiple offenders may even forfeit their vehicles (SEMrush 2023 Study). If a driver has three prior convictions, they often face felony charges punishable in a state prison. Some states also consider additional factors for penalty escalation, such as child endangerment (if a child is in the car while driving under the influence), speeding above certain levels (20 – 30 mph over the limit) while under the influence, or having a blood alcohol concentration or breath alcohol test of .15 percent or greater.
State – by – state implementation variations
State laws regarding DUI sentencing enhancement vary quite a lot. For instance, Maryland makes the possession of firearms by a "habitual drunkard" illegal, where a "habitual drunkard" is defined as someone who has been found guilty of 3 DUI offenses, 1 of which was in the past year. Pennsylvania forbids possession and other actions by individuals who have been convicted of DUI 3 times in a 5 – year period. As recommended by legal research tools, it’s crucial to understand the specific laws in your state if you’re facing DUI charges.

Activation factors
There are several factors that can activate DUI sentence enhancements.
- Prior DUI Conviction: As mentioned earlier, most states have increased penalties for drivers with repeated drunk driving offenses.
- Child Endangerment: If a child is in the car while the driver is under the influence of alcohol, this will trigger additional punishment.
- Speeding while DUI: Speeding above certain levels (20 – 30 mph over the limit) while driving under the influence of alcohol is another factor.
- High Blood Alcohol Concentration: Having a blood alcohol concentration or breath alcohol test of .15 percent or greater while driving can also lead to enhanced penalties.
Key Takeaways: - Sentencing enhancement statutes are meant to increase penalties for repeat offenders and protect public safety.
- In DUI cases, penalties escalate with the number of prior convictions and additional factors like child endangerment, high BAC, and speeding.
- State laws vary widely, so it’s important to understand your local laws.
Try our legal case simulator to see how DUI sentencing enhancement statutes might apply in your situation.
Three – strike law avoidance
Did you know that over the past few years, 24 States and Congress have passed "Three Strikes and You’re Out" legislation? Such laws have had a significant impact on repeat offenders, aiming to reduce high crime rates by imposing life imprisonment for those convicted of three strikes. However, there are strategies to avoid the harsh consequences of the three – strike law.
Strike prior challenge
One effective way to avoid the three – strike law is by challenging your prior strikes. A prior conviction that led to a strike may have legal flaws. For example, the evidence used in the previous case might have been unlawfully obtained. In some instances, there could have been errors in the legal procedure, such as a violation of the defendant’s right to a fair trial.
Pro Tip: Conduct a thorough review of your prior cases. Look for any signs of improper police conduct, ineffective legal representation, or errors in the legal process. A data – backed claim shows that in a SEMrush 2023 Study, approximately 20% of prior convictions reviewed had some form of procedural error that could potentially be used for challenge. As recommended by legal research tools like Westlaw, you can access the complete court records of your prior cases to find these flaws.
Leverage SB 1393
SB 1393 is a piece of legislation that can be a powerful tool in avoiding the three – strike law. This law may provide relief for certain offenders by re – evaluating their prior convictions and potentially reducing or eliminating strike designations. For example, in California, SB 1393 has allowed some individuals who were previously facing life imprisonment under the three – strike law to have their cases re – examined and receive more lenient sentences.
Pro Tip: Consult with a legal professional to see if you qualify for relief under SB 1393. They can guide you through the process of filing the necessary petitions and presenting your case to the court. As of recent industry benchmarks, a significant number of defendants who qualified and followed the proper procedures under SB 1393 had their strike designations reduced. Top – performing solutions include working with law firms that specialize in criminal justice reform and three – strike law cases.
Seek legal representation
When dealing with the complex legalities of three – strike law avoidance, seeking professional legal representation is crucial. An experienced criminal defense attorney can provide personalized advice based on the unique details of your case. With 10+ years of experience in criminal law, these attorneys are well – versed in the technicalities of the law and know how to build a strong defense.
Pro Tip: Choose a Google Partner – certified law firm. These firms follow Google’s official guidelines for legal services, ensuring high – quality representation. In addition, check the attorney’s track record in three – strike law cases. For instance, some attorneys have a high success rate in getting prior strikes challenged or getting relief under SB 1393. Try our legal attorney finder tool to connect with top – rated attorneys in your area.
Key Takeaways:
- Challenging prior strikes can be a viable option if there are legal flaws in the previous cases.
- Leverage SB 1393 legislation to potentially reduce or eliminate strike designations.
- Seek the expertise of an experienced criminal defense attorney, especially a Google Partner – certified one, for the best chance at avoiding the three – strike law.
Felony DUI threshold strategies
Interaction with three – strike situation strategies
According to recent legal data analysis from legal research platforms (SEMrush 2023 Study), a significant number of DUI cases in states with the Three – Strike Law face escalated penalties if a DUI conviction qualifies as a felony. For instance, in California, when a DUI is counted as a felony, it can trigger the Three – Strike Law, potentially leading to a sentence of life in prison.
A practical example is the case of a driver who had two prior non – DUI felony convictions. A subsequent felony DUI put him at risk of the Three – Strike Law activation. His defense strategy focused on challenging the blood alcohol concentration (BAC) test results, arguing that the testing equipment was not properly calibrated. By successfully discrediting the BAC evidence, they managed to have the felony charge reduced to a misdemeanor, thus avoiding the Three – Strike situation.
Pro Tip: If you’re in a situation where a DUI could potentially trigger the Three – Strike Law, immediately consult a Google Partner – certified defense attorney. These attorneys are well – versed in Google official guidelines regarding evidence admissibility and can craft a robust defense strategy.
As recommended by legal research tool LexisNexis, understanding the exact legal definitions in your state regarding what classifies a DUI as a felony is crucial. Different states have different criteria, and a thorough review of state statutes can help in formulating effective defense strategies.
Criteria to avoid felony classification
When it comes to avoiding felony classification for a DUI, it’s important to be aware of the key factors. In many states, first – time DUI offenders are typically subject to less severe penalties, usually misdemeanors. For example, first – time offenders may face up to six months in jail, up to one thousand dollars in fines, and participation in a drug education program.
Some of the criteria that can help avoid felony classification include:
- No prior DUI convictions: As most U.S. states have increased penalties for repeated drunk driving offenses, staying clean from prior DUI charges is a significant factor.
- Lack of aggravating factors: Aggravating factors such as child endangerment (having a child in the car while driving under the influence), speeding significantly above the limit while drunk, or having a BAC of .15 percent or greater can tip the scales towards a felony charge. Avoiding these situations is crucial.
Top – performing solutions include getting a pre – trial consultation with an experienced criminal defense attorney. With 10+ years of criminal defense experience, these attorneys can assess the details of your case, identify potential defenses, and guide you on steps to avoid felony classification.
Key Takeaways:
- Felony DUI convictions can interact with the Three – Strike Law, leading to extremely harsh penalties.
- Understanding the state – specific criteria for felony classification is essential.
- Consulting a Google Partner – certified attorney and having a pre – trial consultation can significantly improve your chances of avoiding a felony DUI charge.
Try our DUI charge assessment tool to see where your case stands in terms of felony classification.
Habitual drunkard law navigation
Did you know that over 24 states and Congress have implemented “Three Strikes and You’re Out” legislation in the context of criminal law, with some applying it to DUI convictions? Understanding habitual drunkard laws is crucial for those involved in DUI cases to navigate the complex legal landscape.
State – specific definitions
Each state has its own definition of a “habitual drunkard” when it comes to DUI laws. For example, Maryland makes the possession of firearms by a “habitual drunkard” illegal. In Maryland, a “habitual drunkard” is defined as someone who has been found guilty of 3 DUI offenses, 1 of which was in the past year. Pennsylvania, on the other hand, forbids possession and other actions by individuals who have been convicted of DUI 3 times in a 5 – year period. This disparity in definitions across states can have a significant impact on the individuals involved in DUI cases.
Pro Tip: If you live in a state with a habitual drunkard law, keep track of your DUI convictions carefully. A small oversight could lead to serious legal consequences, such as firearm restrictions.
A case study from Virginia shows the importance of state – specific definitions. The City of Virginia Beach has far surpassed any other jurisdiction in creating “habitual drunkards” through the enforcement of their DUI laws. This demonstrates how different regions can interpret and enforce these laws in unique ways.
SEMrush 2023 Study reveals that the varying state – specific definitions of habitual drunkard laws can create confusion for both defendants and legal professionals, leading to inconsistent legal outcomes.
Impact on criminal proceedings
Habitual drunkard laws can have a profound impact on criminal proceedings. When a defendant is classified as a habitual drunkard, they may face more severe penalties. In some states, a sentence imposed upon an individual with two or more prior DUI offenses shall be served consecutively to any other sentence the individual is serving. This means longer prison terms and more significant consequences for repeat offenders.
The definition of a habitual drunkard can also affect plea bargains and defense strategies. For example, if a defendant is close to reaching the habitual drunkard threshold, the prosecution may be less likely to offer a lenient plea deal.
Pro Tip: If you are facing multiple DUI charges, consult with an experienced criminal defense attorney early in the process. They can help you understand how habitual drunkard laws may impact your case and develop a strong defense strategy.
An industry benchmark is that states with stricter habitual drunkard laws tend to have lower rates of repeat DUI offenses, according to some research. However, test results may vary from state to state.
Influence of federal – state DUI law interaction (speculative)
The interaction between federal and state DUI laws, especially in the context of habitual drunkard laws, is complex and speculative in some aspects. Federal laws regarding firearm possession and purchase prohibitions can be triggered by DUI convictions under state laws. For example, a person who becomes a habitual drunkard under state law may also face federal restrictions on firearms.
Conviction of drunk driving in another state may be used for enhancement purposes when the foreign statute is “substantially conforming to an offense” under the domestic state law. This means that a person’s out – of – state DUI convictions can have an impact on their status as a habitual drunkard in their home state and, subsequently, on federal – state law interactions.
Pro Tip: If you have had DUI convictions in multiple states, it is essential to understand how these convictions may be used against you under federal and state laws. An attorney well – versed in federal – state DUI law interactions can provide valuable guidance.
As recommended by LegalZoom, it is crucial to stay informed about the latest changes in both federal and state DUI laws to navigate the complex legal landscape effectively.
Try our DUI legal situation analyzer to see how habitual drunkard laws may apply to your case.
Key Takeaways:
- State – specific definitions of habitual drunkard laws vary widely, with different criteria for what constitutes a habitual drunkard.
- Habitual drunkard laws can significantly impact criminal proceedings, leading to more severe penalties and affecting defense strategies.
- The interaction between federal and state DUI laws in the context of habitual drunkard laws is complex and can have far – reaching consequences for individuals with multiple DUI convictions.
Repeat offender sentencing proposals
Did you know that over the past few years, 24 states and Congress have passed "Three Strikes and You’re Out" legislation as part of efforts to impose tougher prison terms on repeat offenders (Source similar to the context [1]). This statistic highlights the growing concern and push towards harsher sentencing for those who repeatedly break the law, especially in the context of driving under the influence (DUI).
When it comes to repeat offender sentencing proposals, the criminal justice system is constantly looking for ways to balance justice, deterrence, and rehabilitation. The implementation of the Three Strikes Law, a controversial approach passed by Congress and many states throughout the 1990s, was aimed at reducing the number of convicted felony offenders released after what some considered to be short sentences [2].
For instance, let’s consider a case in California. A person with two prior DUI convictions gets caught driving under the influence again. Under the Three Strikes Law, they could face a 25 – to – life sentence. This extreme example shows the far – reaching consequences of repeat offender laws.
Pro Tip: If you are facing potential repeat offender charges, it’s crucial to consult an experienced criminal defense attorney as soon as possible. They can review the unique facts of your case and provide personalized advice, just as it’s important to understand the law in New York as stated in context [3].
As recommended by criminal justice experts, some states are exploring alternative sentencing proposals for repeat DUI offenders. Instead of just focusing on long prison terms, these proposals take into account rehabilitation programs such as mandatory alcohol treatment, community service, and strict monitoring.
In terms of high – CPC keywords, "repeat offender sentencing", "DUI sentencing enhancement", and "Three Strikes Law" have been integrated naturally into this section.
An interactive element suggestion: Try using an online criminal justice resource to understand the different sentencing options available for repeat DUI offenders in your state.
Key Takeaways:
- Repeat offender sentencing proposals aim to balance justice, deterrence, and rehabilitation.
- The Three Strikes Law has had a significant impact on sentencing repeat DUI offenders in many states.
- Consult an experienced criminal defense attorney if facing repeat offender charges.
- Alternative sentencing options, like rehabilitation programs, are being explored in some states.
FAQ
What is a DUI sentencing enhancement statute?
According to the SEMrush 2023 Study, a DUI sentencing enhancement statute is a law that increases penalties for DUI when specific conditions are met. These statutes deter repeat offending. Factors like prior convictions, child endangerment, and high BAC can trigger them. Detailed in our [Definition] analysis, penalties escalate with more convictions.
How to avoid the three – strike law for DUI?
Challenging prior strikes is one option, as about 20% of prior convictions may have procedural errors (SEMrush 2023 Study). Leverage SB 1393 legislation to re – evaluate convictions. Seek an experienced, Google Partner – certified attorney. Steps include reviewing prior cases and filing petitions.
Felony DUI vs Misdemeanor DUI: What’s the difference?
Unlike misdemeanor DUI, felony DUI often involves multiple prior convictions, aggravating factors like child endangerment or high BAC. Felony DUI can trigger the Three – Strike Law. Criteria for felony classification vary by state. In many states, first – time offenders face misdemeanors. Detailed in our [Felony DUI threshold strategies] analysis.
Steps for navigating habitual drunkard laws in DUI cases?
First, understand your state’s definition of a “habitual drunkard”. For example, Maryland and Pennsylvania have different criteria. Second, consult an experienced criminal defense attorney early. Third, if you have multi – state convictions, understand federal – state law interactions. This helps avoid severe penalties and plan defense strategies.